
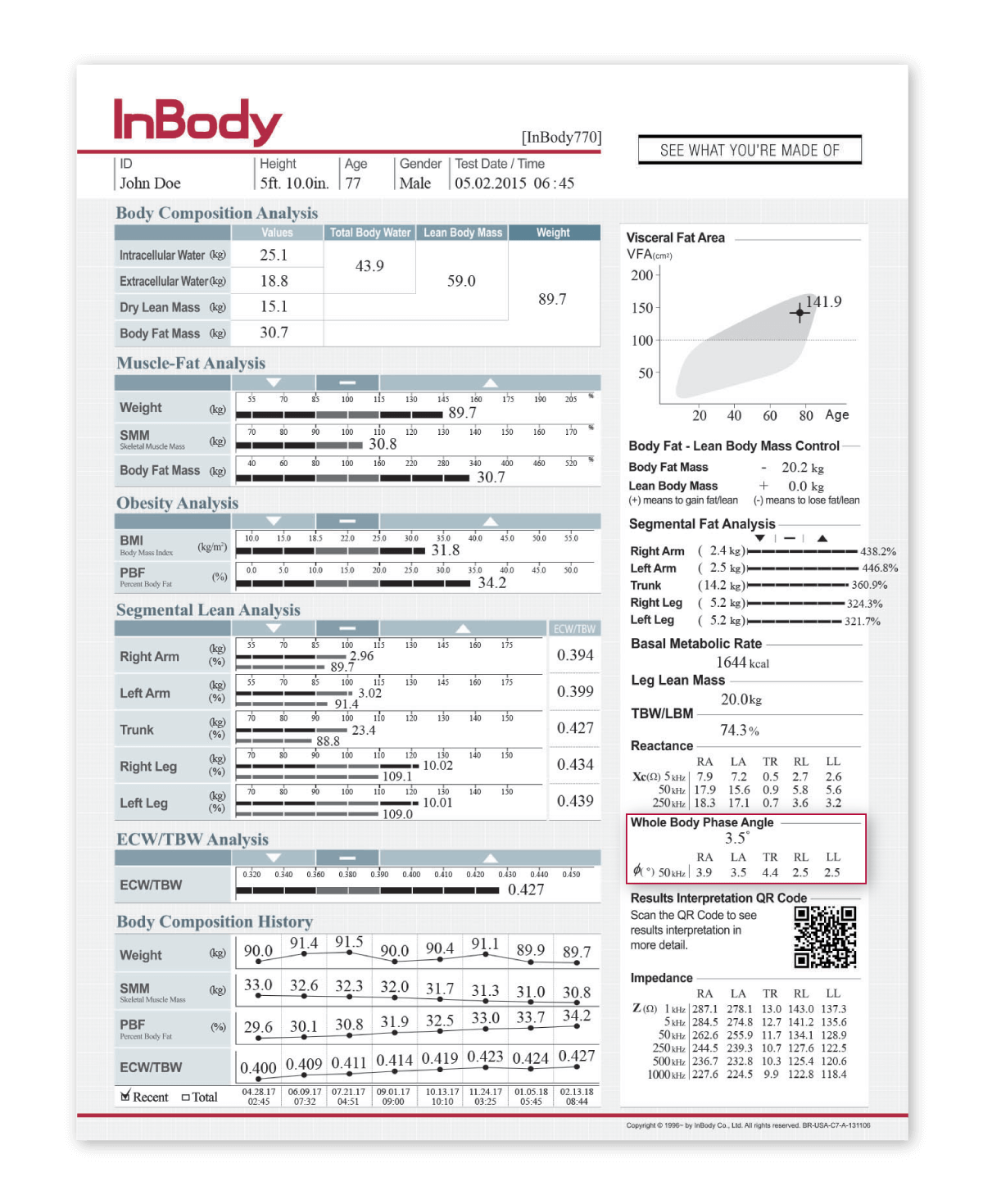
Body composition is important for understanding a patient’s cardiovascular health. High blood volume, increased water levels in the body, strains on the heart are all issues that stem from conditions like obesity. BMI is commonly used to determine a patient’s risk for cardiovascular disease; however, BMI overlooks a patients’ visceral fat that is often linked to a higher risk for cardiovascular risk. By using this method, doctors cannot determine how much of a patient’s body is muscle or fat.
On the other hand, body composition analysis differentiates between a patient’s muscle, fat, and water levels. Studies have proven InBody DSM-BIA body composition analyzers are an effective tool for treating patients with cardiovascular disease and improving surgical outcomes. InBody devices ensure cardiology professionals can be certain that the outputs generated accurately reflect changes within the patient.
In less than 60 seconds, cardiology professionals receive an InBody Result Sheet (body composition printout) that can aid in:
“EI determined by BIA is a useful predictor of the amount of weight reduction needed to reach dry weight…in HF patients..”
“a significantly higher percentage of participants with VFA ≥100 cm2 had diabetes, obesity, hypertension, hypertriglyceridemia and hypo-HDL cholesterolemia..”
“Preoperative low PA is an accurate marker of malnutrition and an independent predictor of adverse postoperative outcomes…We recommend using it to detect malnutrition in the cardiac surgery population.”




 DIRECT SEGMENTAL MEASUREMENT (DSM)
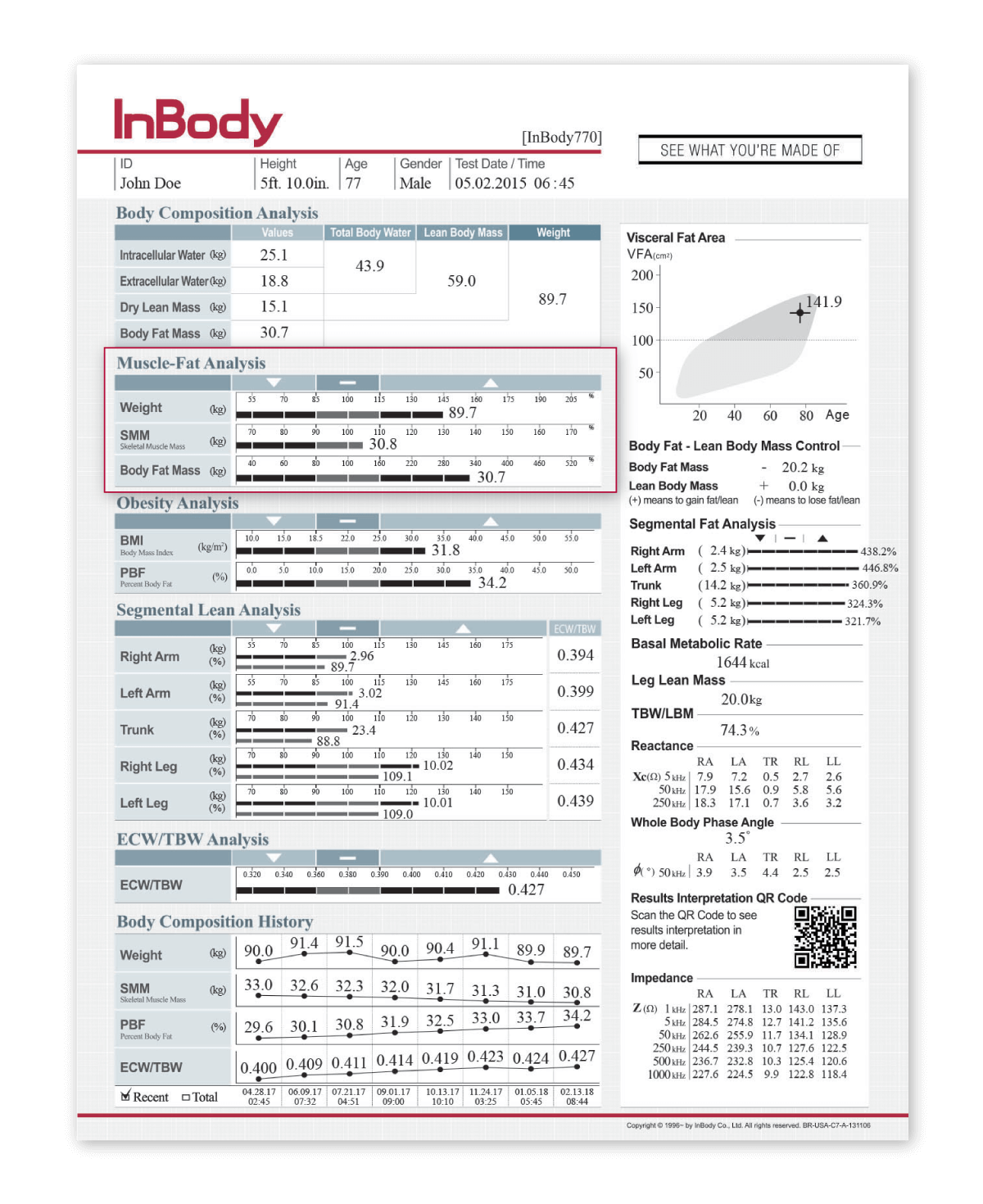
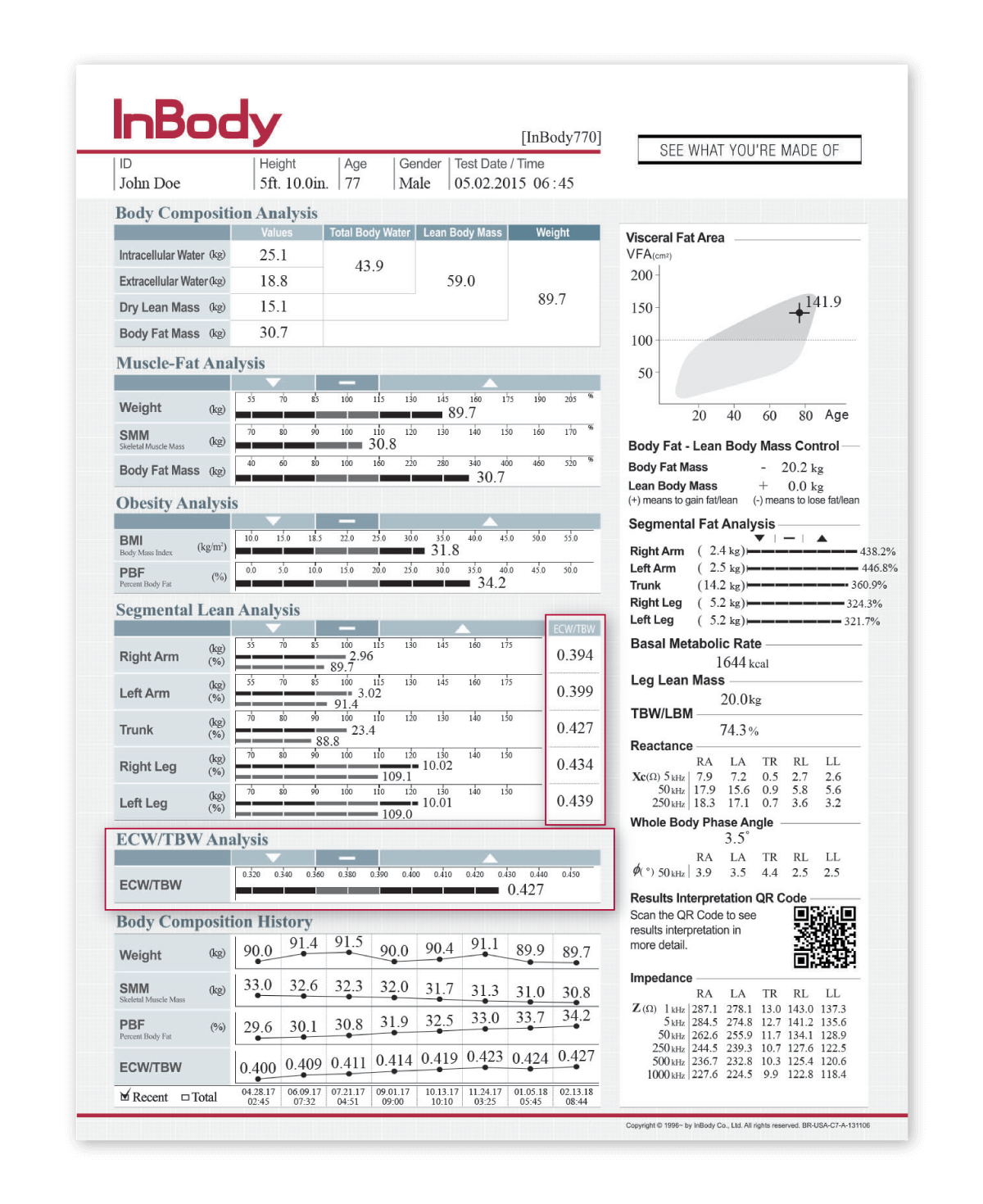
DIRECT SEGMENTAL MEASUREMENT (DSM)Direct Segmental Measurement (DSM) measures water, muscle mass and fat mass in the five body segments: right arm, left arm, left leg, right leg and trunk. By measuring each segment of the body separately, the InBody provides an in-depth analysis of the patient’s muscle-fat and fluid balance in each segment independently. Identifying the patient’s lean and fat distribution allows a better assessment of associated health risks, and segmental ECW/TBW can be used to identify systemic or localized inflammation resulting from obesity
 MULTIPLE FREQUENCIES
MULTIPLE FREQUENCIESInBody devices utilize multiple frequencies to measure body water more accurately than commonly-used methods such as weight changes or pitting edema scores. These high and low frequencies are able to measure both intra- and extracellular water, producing more precise measurements of body water compartments. Having an accurate measure of the different water compartments can indicate fluid imbalances or water retention stemming from circulation issues and can be used to monitor changes in fluid balance following diuretic use.
 8 POINT TACTILE ELECTRODES
8 POINT TACTILE ELECTRODESInBody devices use 8-Point Tactile Electrodes to ensure that measurements always start in the same place, test after test. This technology creates precise and reproducible results, ensuring the results professionals are seeing are genuine changes happening to their patient and are not due to error.
 NO EMPIRICAL ESTIMATIONS
NO EMPIRICAL ESTIMATIONSInBody devices do not rely on empirical estimations to predict results. Empirical data such as age, gender and ethnicity does not change an individual’s results, an important factor for cardiology professionals as heart failure affects each patient differently. By not relying on pre-loaded data, cardiology professionals know that the data they are obtaining on their patient is based on that patient alone. Therefore, any changes that are happening to a patient reflects a genuine change in their body composition.

