
Early identification of disease onset is imperative for patient care by providing practitioners with tools to develop interventions to improve long-term health outcomes. InBody devices are space-efficient, are easy to incorporate into patient screenings and the data can easily be implemented into patient management software. The InBody test provides a comprehensive printout that serves as an ideal educational tool for engaging patients in understanding health risk management and reduction.
In less than 60 seconds, an InBody Test can provide easy-to-understand, accurate, and objective measurements to evaluate a patient’s disease risk. Doctors and nurses can use the InBody to:
“Low relative muscle mass was associated with an increased prevalence for subclinical coronary artery disease and the degree of coronary artery calcification in a dose-dependent manner..”
“Additionally, the assessment of the body composition parameters provides additional information on cardiovascular risk and … play an important role in the health state evaluation..”
“It (BIA) has been shown that it can reliably reflect body composition and associate with patient’s nutritional statuses or clinical outcomes..”

Due to the rising prevalence of sedentary, inactive lifestyles, patients are more likely to become frail or suffer from injuries leading to reduced mobility. Evaluate lean mass distribution and identify imbalances to prevent or treat sarcopenia and improve physical function.
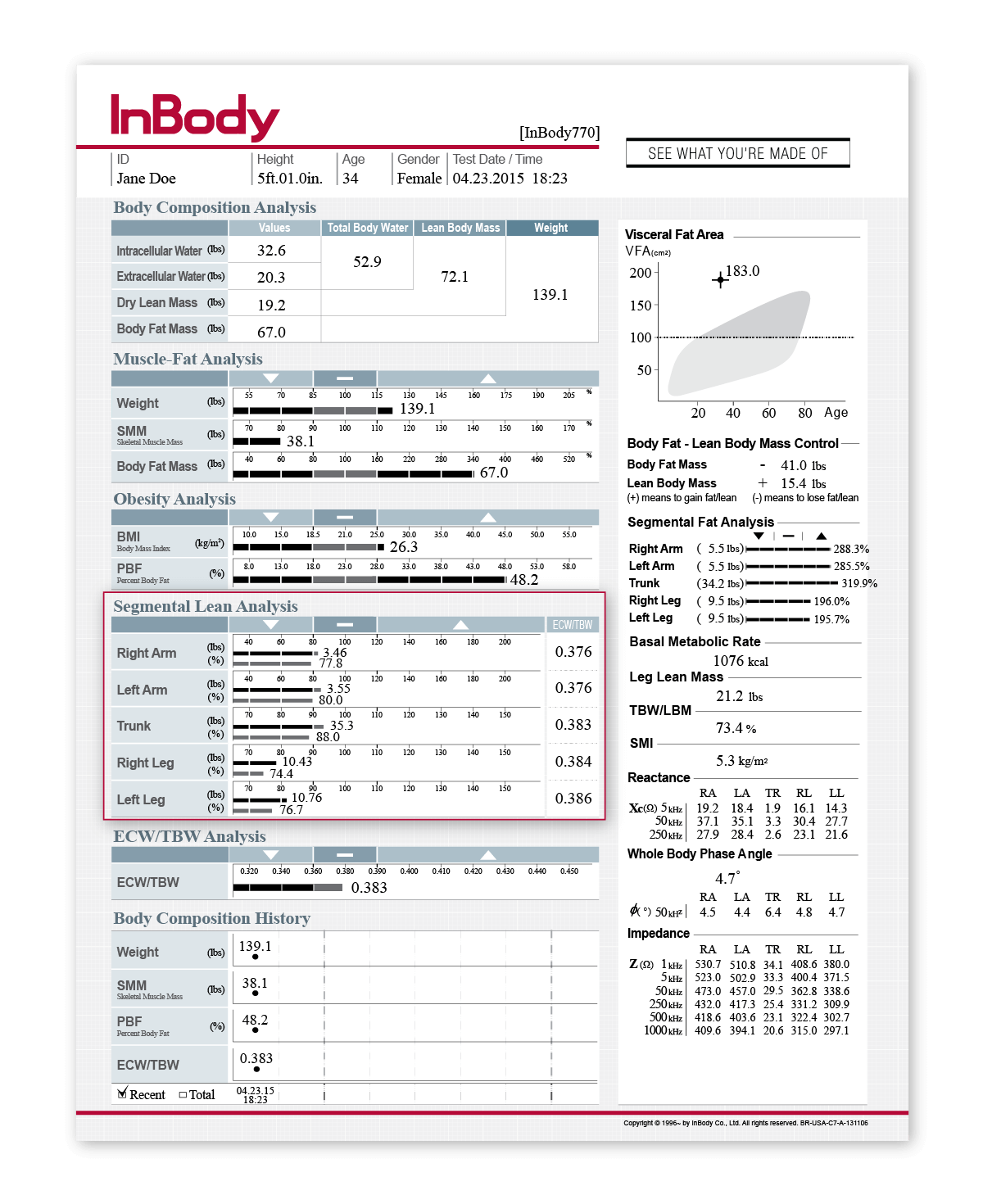
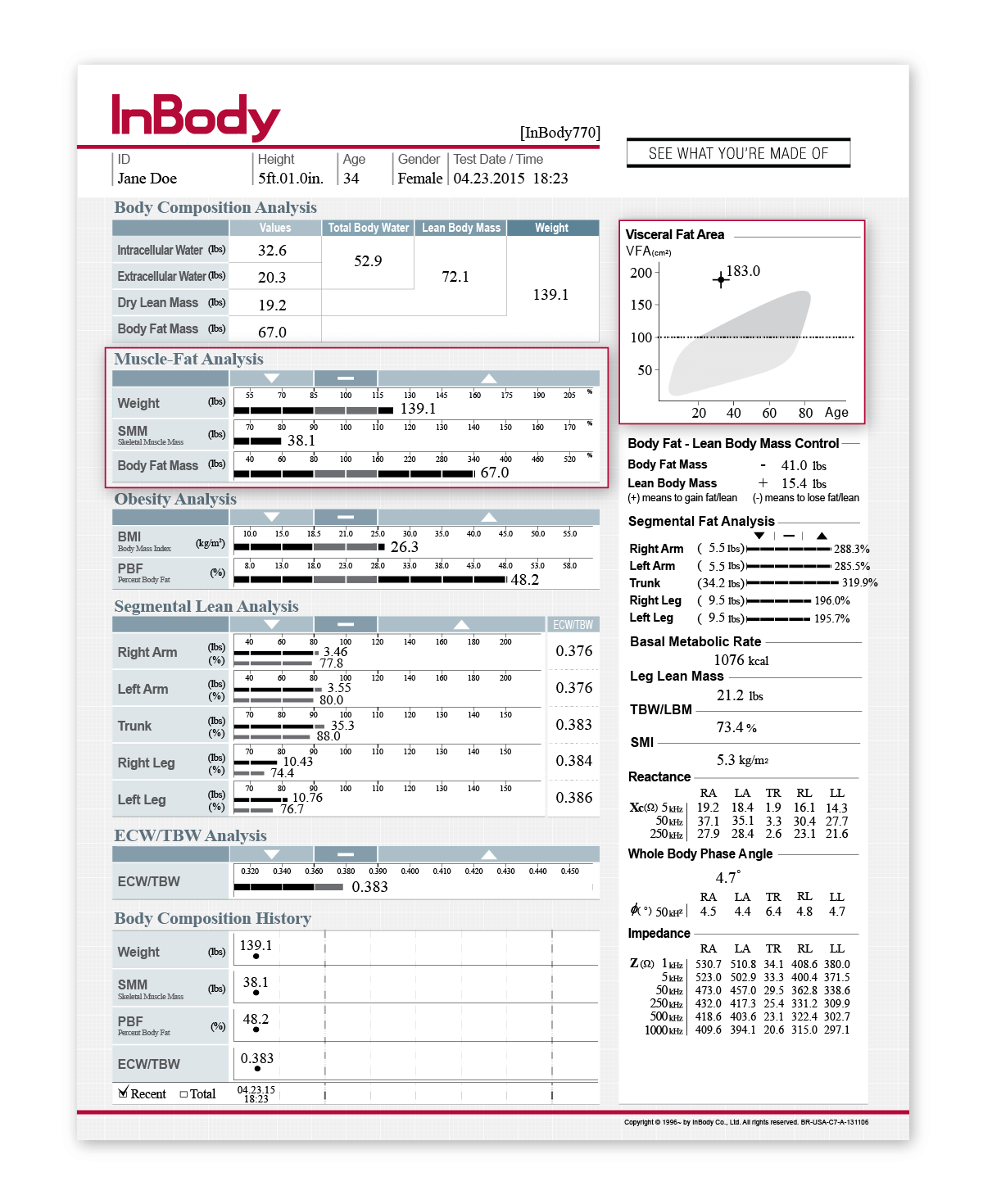
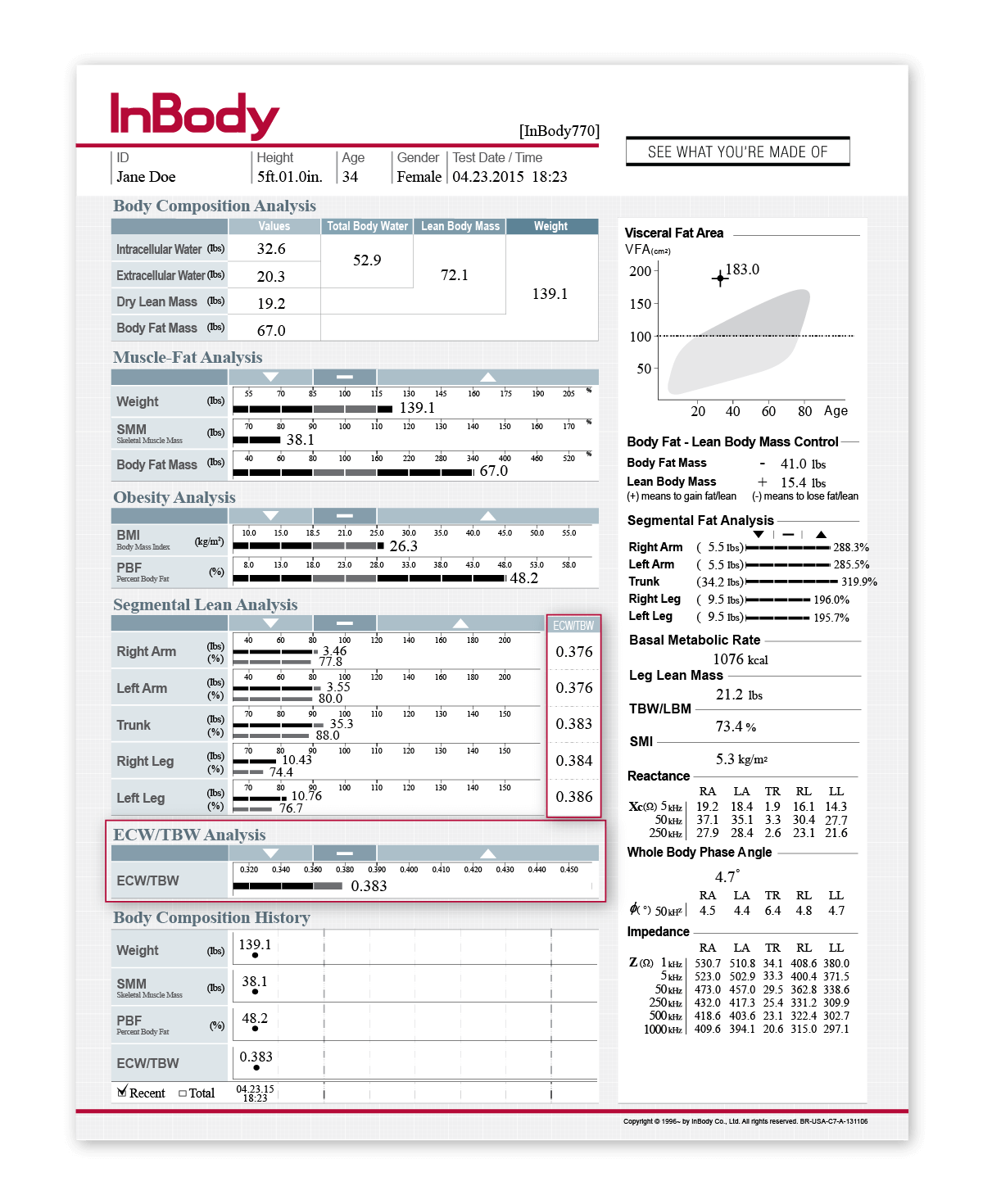
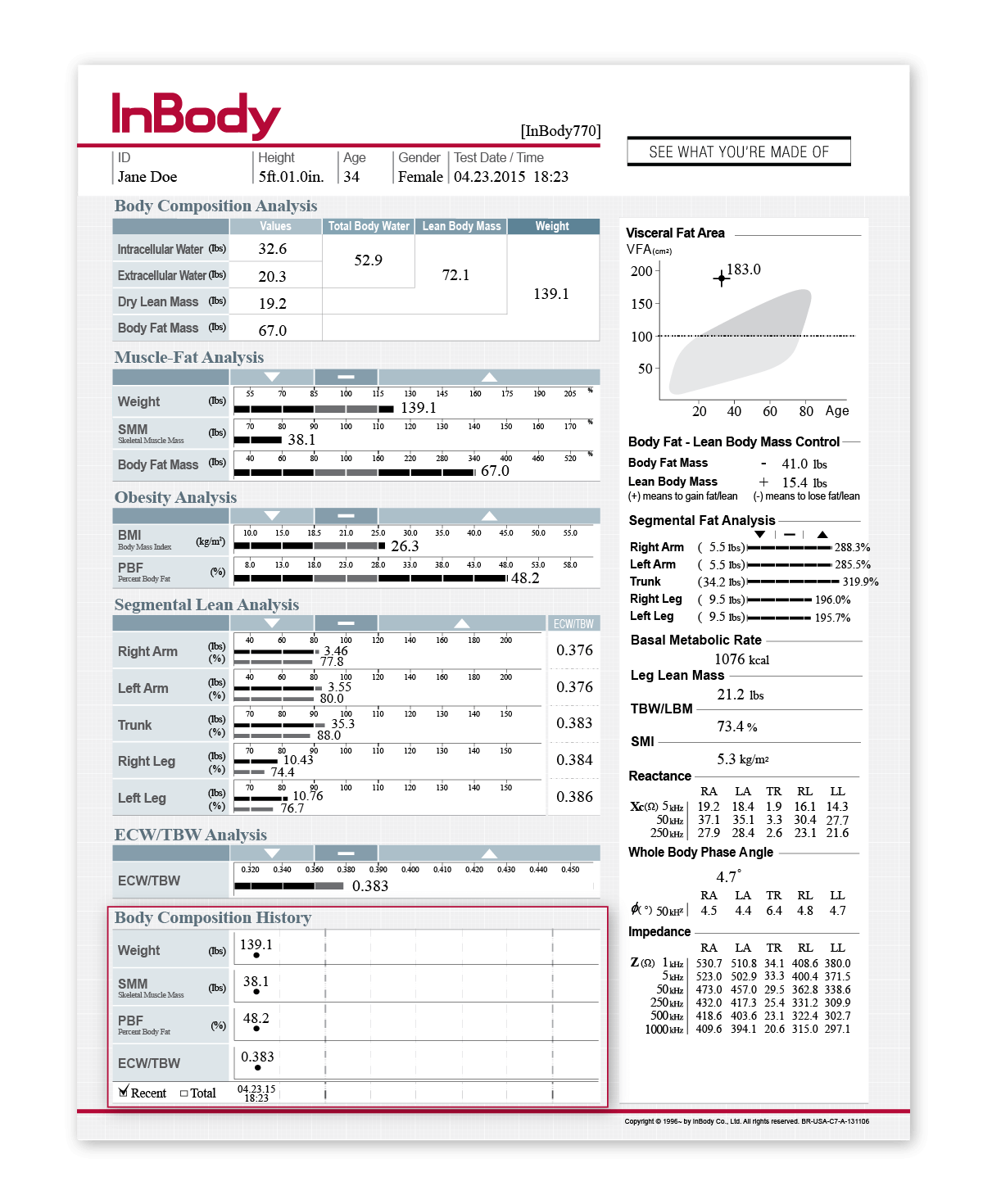
Chronic inactivity and poor diet have deleterious effects on body composition, eventually impacting physical function and quality of life. Sedentary lifestyles cause degenerative loss of muscle mass, increasing risk of falls and mobility issues as a patient ages. The InBody measures lean body mass in each segment of the body separately, allowing identification of insufficient development or muscular imbalances. These objective measures of lean mass distribution and development provide practitioners with information to identify increased risk of frailty and develop targeted recommendations for maintaining functional mobility.

Doctors rely on the use of BMI to assess health risk. Assess muscle and fat composition separately to evaluate to nutrition status and examine the patient’s current health risks.
Measuring body composition allows the practitioner to break body weight down into separate compartments of muscle and fat mass, both independent contributors to functional status, insulin sensitivity, and health risk. Identifying patients who have low muscle mass or a combination of low muscle and high fat mass (sarcopenic obesity) can help provide earlier interventions for reducing cardiometabolic risk.
Excess fat mass can also be easily identified across the whole body, while separate assessment of visceral fat mass can help practitioners further assess patient-specific health risks. By using the Muscle-Fat Analysis and Visceral Fat sections of the InBody Results Sheet, the physician will be able to perform a more specific health risk assessment.

Although disease risk is often associated with inflammation, diagnostic markers of fluid retention and inflammation are time consuming and inconvenient. InBody’s technology is able to precisely track fluid changes across the body to understand the cause of imbalanced fluid levels.
InBody effectively distinguishes water in the intracellular (ICW; within the tissues) and extracellular (ECW; within the blood and interstitial fluids) compartments that make up total body water (TBW). The Edema Index, based on the ratio between ECW and TBW (ECW/TBW), can be used to distinguish fluid imbalances resulting from malnutrition or edema. Managing increases in Edema Index is a priority for improving patient outcomes.
Due to the high water content of muscles, loss of muscle mass causes a reduction in ICW and results in an increased Edema Index. Thus, the Edema Index can be used to identify muscle loss and its link to associated health conditions. Since cardiovascular disease is associated with increased systemic inflammation, progressing fluid imbalances, the Edema Index can be used to identify and monitor long-term fluid retention, which may lead to comorbidities such as renal or cardiac dysfunction. Monitoring the Edema Index can help physicians understand disease-related fluid imbalances more accurately.

General practitioners do not see patients enough to subjectively monitor critical changes to patient health through tools such as BMI or physical assessments. By tracking body composition history, doctors can detect changes that can aid in patient education and earlier detection of disease.
It is often difficult to detect subclinical changes to a patient’s health status, such as muscle loss and inflammation, with a physical exam. These changes are often minimal in early stages of disease and are combined with an increase in fat mass or fluid accumulation, which may mask indications of disease or result in an underestimation the severity of the condition when looking at weight alone. Tracking changes to muscle mass, fat mass, and the Edema Index allows health care providers to educate patients regarding their health risks and set goals to improve body composition and overall health.

 DIRECT SEGMENTAL MEASUREMENT (DSM)
DIRECT SEGMENTAL MEASUREMENT (DSM)Direct Segmental Measurement (DSM) measures water, muscle mass and fat mass in the five body segments: right arm, left arm, left leg, right leg and trunk. By measuring each segment of the body separately, the InBody provides an in-depth analysis of the patient’s muscle-fat and fluid balance in each segment independently. Identifying the patient’s lean and fat distribution allows a better assessment of associated health risks, and segmental ECW/TBW can be used to identify systemic or localized inflammation resulting from obesity
 MULTIPLE FREQUENCIES
MULTIPLE FREQUENCIESInBody devices use multiple frequencies to measure body water more accurately than physical examinations. These high and low frequencies are able to measure both intra- and extracellular water, producing more precise measurements of body water compartments. Having an accurate measure of the different water compartments can indicate fluid imbalances or water retention stemming from circulation issues and can be used to monitor changes in fluid balance to monitor disease progression.
 8 POINT TACTILE ELECTRODES
8 POINT TACTILE ELECTRODESInBody devices used 8-Point Tactile Electrodes to ensure that measurements always start in the same place, test after test. This technology creates precise and reproducible results, ensuring that the changes to the results over time are comparable and genuine.
 NO EMPIRICAL ESTIMATIONS
NO EMPIRICAL ESTIMATIONSInBody devices do not rely on empirical estimations to predict results. Age, gender and ethnicity do not contribute to calculating an individual’s results, an important factor for general practitioners as every patient is unique. By not relying on empirical estimations, general practitioners can be confident that the data they are obtaining on their patient is reflective of that patient alone. Therefore, any changes that are happening to a patient reflects a genuine change in their body composition.

