
InBody devices provide a quick, easy, non-invasive, and precise method for assessing health risks and the effects of interventions. In less than 60 seconds, the InBody Test can be used to:
“Here, we found that phase angle was a predictor of survival independent of many established objective laboratory markers, such as hypoalbuminemia, leukocytosis, neutrophil-to-leukocyte ratio, and elevated lactate dehydrogenase.”
“SMI was a significant independent prognostic factor for cancer-related deaths in patients with gastric or colorectal cancer who had undergone surgery, and a marginally independent factor that negatively contributed to overall survival in these patients.”
“In conclusion, gastric cancer patients, whether cachectic or non-cachectic, have decreased serum leptin levels, which may depend not only on the fat mass percentage but also GH and insulin.”




 DIRECT SEGMENTAL MEASUREMENT (DSM)
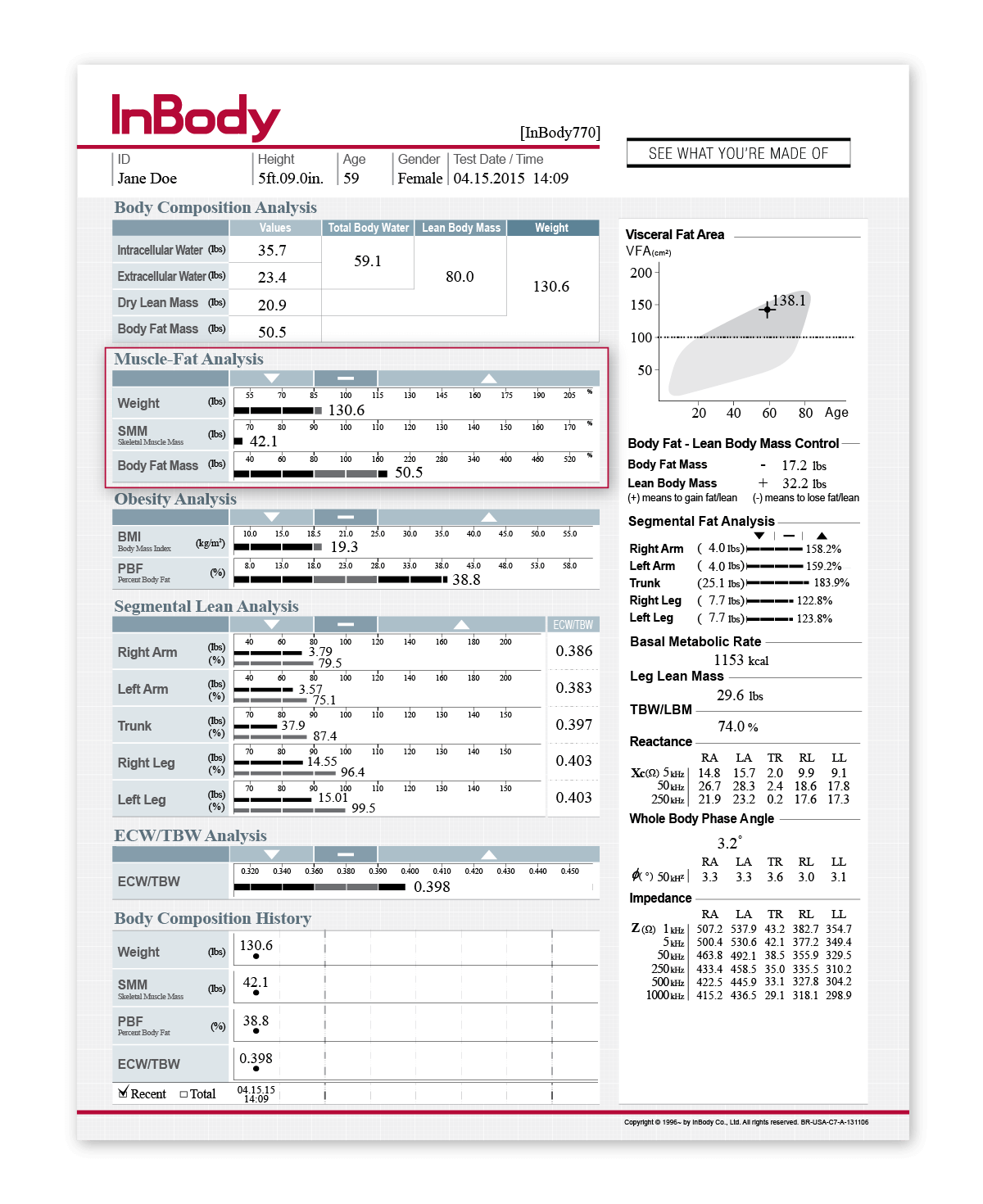
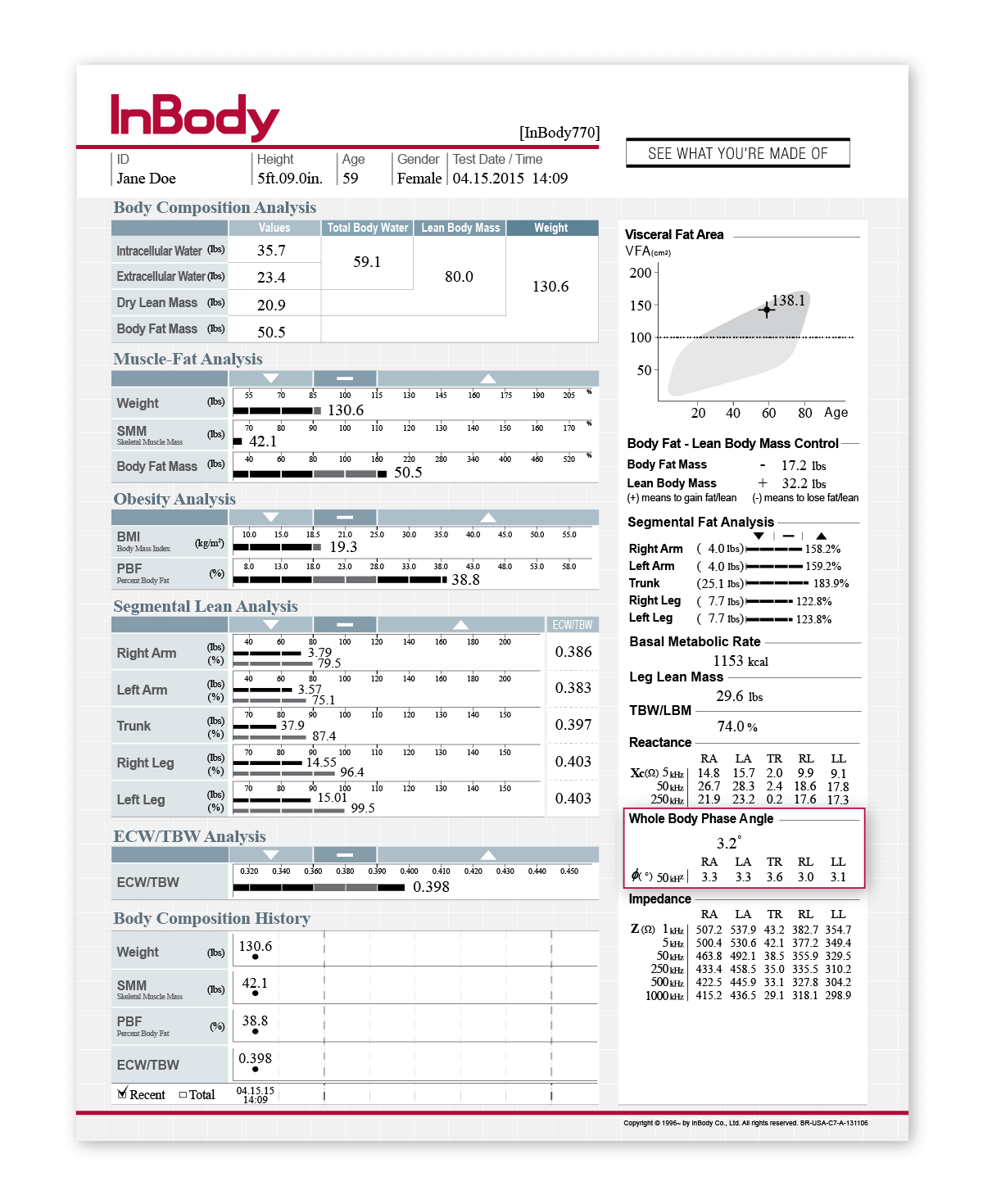
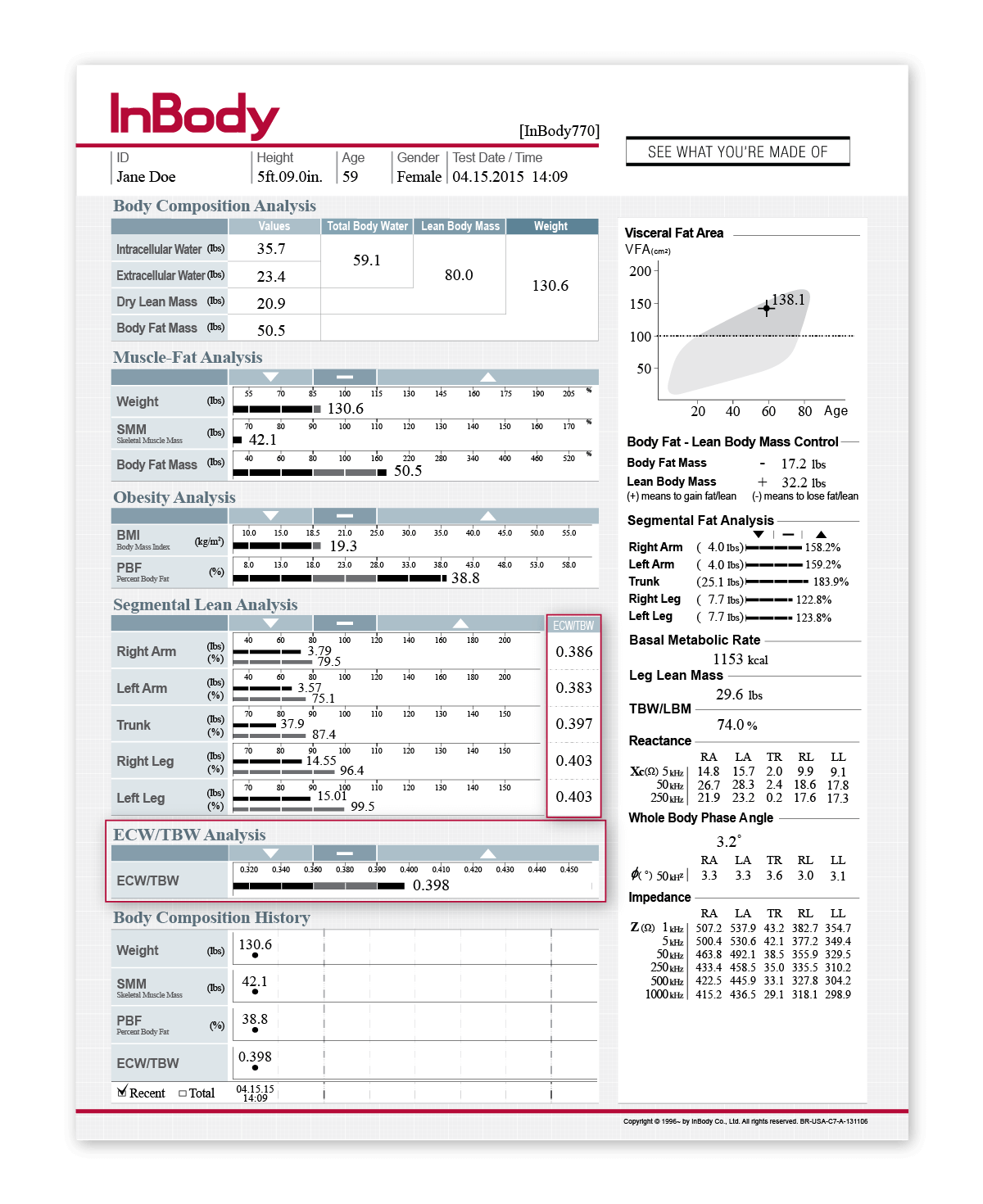
DIRECT SEGMENTAL MEASUREMENT (DSM)Direct Segmental Measurement allows for muscle and fat mass readings in each segment of the body: right arm, left arm, left leg, right leg and trunk. By measuring each segment of the body separately, the InBody is able to provide an in-depth analysis of a patient’s fluid balance for each region. These outputs include intracellular water, extracellular water, and ECW/TBW ratio. With objective measures of body water, including intracellular water, extracellular water, and the Edema Index (ECW/TBW), localized or systemic edema can be identified and tracked over time.
 MULTIPLE FREQUENCIES
MULTIPLE FREQUENCIESInBody devices use multiple frequencies to measure body water more accurately than commonly used methods like pitting edema scores. These high and low frequencies are able to measure both intra- and extracellular water, producing quantified and objective measurements of body water compartments. Accurate measures of the different water compartments can indicate fluid imbalances or water retention stemming from circulation issues and can be used to monitor changes in fluid balance following treatment.
 8 POINT TACTILE ELECTRODES
8 POINT TACTILE ELECTRODESInBody uses 8-Point Tactile Electrodes to ensure that measurements always start in the same place, test after test. This technology creates precise and reproducible results, ensuring that the changes professionals are seeing in their patients are accurate and comparable.
 NO EMPIRICAL ESTIMATIONS
NO EMPIRICAL ESTIMATIONSInBody devices do not rely on empirical, or pre-loaded, data to predict results. Age, gender, and ethnicity do not contribute to an individual’s results, an important factor for oncology professionals as cancer affects each patient differently. By not relying on pre-loaded data, oncology professionals can be confident that the data they are obtaining on their patient is reflective of that patient alone. Therefore, any changes that are happening to a patient reflects a genuine change in their body composition.

